Using Stem Cells to Reverse Aging
Reprogramming our developmental time table to go backwards!
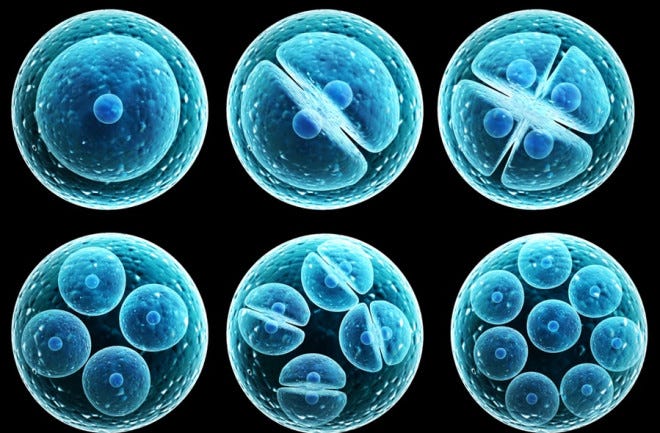
Stem cells are amazing precursors to all of our specialized cells such as eye, bicep, gut and skin. I imagine them like embryos, waiting to be tapped to develop into one of the myriad specialist cells of the body. Recall that each of us developed from a single fertilized egg, the ultimate stem cell, that gave rise to our trillions of mature cells. Early on during embryonic development, it’s possible to take one of a total of, say, 32 or 64 cells; each of these in the right conditions could give rise to another embryo capable of developing into a fully functional individual. These so-called embryonic stem cells raised a lot of hopes a few decades ago for regenerative possibilities in our aging bodies. Imagine taking one of those cells and coaxing it to develop into a new heart or kidney for someone needing a transplanted organ, or a new knee for those of us whose knees are wearing out.
Politics shut down that line of research. But scientists later discovered that virtually all tissue types in our adult bodies have reservoirs of their own stem cells that, though not capable of developing into any type of cell, can develop into different cells characteristic of their home tissue. Even our brains have stem cells, something that was long denied. So, theoretically, if these so-called ‘pluripotent’ cells (as opposed to the ‘totipotent cells of the early embryo) could be harvested and coaxed into growing in the lab, we could still have hearts or kidneys or knees, and ideally, grown from our own cells so no problems with transplant rejection.
Not so easy to find and harvest these cells, let alone figure out what conditions would encourage them to develop into a new organ. But scientists persevered. In 2012 Shinya Yamanaka received the Nobel Prize for identifying 4 genes in mice that could turn a mature or specialized cell to an immature state. When these genes are added to an adult cell, it regresses to an unspecialized form, i.e. a stem cell. This ‘induced stem cell’ can then develop into various tissue types. This work was done first in mice, but has since been replicated in many other animals including humans.
These 4 genes, known as Yamanaka factors, suggest the possibility to reverse aging in the adult body. Early work along in this area showed that one of the 4 genes promotes cancer, but by leaving that one out, and expressing the other 3 (called OSK – the acronym represents the name of each gene), it was possible to reverse aging in some tissues in mice.
In a remarkable experiment in mice whose optic nerves were damaged causing blindness, adding the OSK factors led to regrowth of the nerves and restoration of vision. Many other tissues, including brain tissue, kidney, and muscle, have now been reprogrammed without causing cancer. Activation of OSK throughout the entire body of mice extends their lifespan.
Although it’s way too early to translate these findings into us aging humans, they suggest the possibility of a ‘re-set’, of what’s called the epigenome. Sorry but I have to introduce this bit of jargon, which is permeating the aging field. (Yet another topic to return to!) Epi- means above or next to, and in the context of the chromosomes, where genes are located, refers to chemical tags attached to the DNA of genes, that act as on or off switches. These tags are added or subtracted through life, causing activation or inhibition of individual genes, which can ultimately contribute to health or disease. Here’s a good visual of epigenetic action:
If you want to dig deeper, you can hear David Sinclair, a Harvard researcher and one of the main developers of the reprogramming approach discuss using OSK in this clip:
The OSK method relies on the delivery of genetic material (the OSK factors, or proteins that activate them) to target tissues. How do you target these factors to the chromosome? This is the stuff of gene therapy and relies on methods such as using a virus to deliver the gene(s). Needless to say, injecting viruses into people is not an easy fix. Not only is it expensive to design and build this kind of system (you have to disable any potential disease-causing genes of the virus and then get the genes you want to deliver into the viral genome), but there are safety concerns associated with the introduction of genetic material into the body.
Current research into reprogramming has shifted to developing a chemical treatment to mimic OSK’s rejuvenating effects. This approach is way more complicated than using a delivery system, because in order to design a chemical you have to understand how the OSK factors work their magic. Still not clear, but various clues exist and are being explored. The scientists are optimistic, but I’m not holding my breath.


I am waiting for the stem cell that can be used in the pancreas to make insulin, I guess it would mimic the beta cells.